20 Dec 2016
We offer our vision of the impact of solar storms on the human body, its circulatory system and its ongoing excess electricity as one of the possible causes of stroke: loss of brain tissue own electricity.

Created nationwide stroke centers, of course, good for the people affected by this disease, but in our opinion and according to the British and Swedish researchers, it is necessary to create a Pre-stroke centers where prevention will be patient in order to prevent a stroke. The relatively small expenditure on prevention will save a lot of money spent now on the treatment and rehabilitation of stroke patients. To implement this direction in the prevention of this terrible disease should already have clinics dedicated service in the face of the doctor neurologist trained in the diagnosis Pre-stroke conditions, knowing thoroughly symptoms begin to crash.
By the symptoms pre-stroke we consider include:
- Venous stasis in the vessels of the brain;
- Growing hypertension in the arterial vessels of the brain.
This issue is unexplored, is available in the arsenal of medical equipment makes it impossible to confidently identify the early stages of cerebral circulation. The only long-practiced eye fundus study can help identify initial changes in cerebral blood flow - a spasm of arteries and venous stasis retinal vascular eye. Since the fundus a person eats from the end branches of the internal carotid artery, and blood vessels have a common innervation to the carotid artery, it allows us to understand and explain the uniformity of the reactions of intracranial vessels and the vessels of the fundus. It is also known that the very short-term cessation of blood circulation in the brain leads to irreversible changes in the nerve cells.
N.A.Nadzharyan (1948.) Studied the effect of stimulation of the auditory, visual and olfactory analyzers of blood circulation in the brain noticed that the change in the lumen of the artery of the brain is made possible by the rapid expulsion of blood from the venous system of the brain vessels. In addition, the occurrence of intense pulsation of cerebral arteries associated with rhythmic rises in intracranial pressure.
Modern ultrasound devices, showing blood flow in the vessels of the head, make it possible to fix the rate of blood flow through the arteries and its variation in certain clinical situations. This makes it possible to identify the group of patients with the slowing of blood flow, which shows the study of blood viscosity parameter is a marker of possible thrombotic events. However, ultrasound is not able to detect venous stasis.
The necessary equipment is capable of measuring the amount of the incoming blood and the amount of flowing blood veins in the brain blood flow system at a particular time, which will allow to diagnose it, venous stasis, which prevents the normal circulation of the blood, with all its consequences, leading up to the thrombus formation in the cerebral arteries with subsequent cerebral ischemia. And so will enable to carry out the necessary pre-treatment in order to eliminate venous congestion, which ultimately leads also to brain edema.
More N. Cybulski (1885) method of determining the rate of blood flow in the arteries, called them photo-hemo-tachometer gives an indication of peripheral resistance to blood flow of intracranial vessels (the so-called cerebrovascular resistance, increasing in Pre-stroke conditions) has been developed. To overcome these conditions, there are three options for reducing the resistance to blood flow. The first - an increase of oxygen in the tissue, compensating its lack (due to poor blood flow). II - increase the exchange surface, the change in blood flow rate through the capillary opening or reducing blood viscosity. And the third - increasing oxygen conductivity of the erythrocyte plasma into the tissue.
The arteries in a person's blood pressure of 80-95 mmHg, in the capillaries is reduced by 20-45 mm Hg, about mitochondria inside the cells of the tissue is only 1-3 mm Hg.
As blood - highly structured, non-Newtonian fluid flowing in a pulsating mode, the vessels - elastic tubes with variable cross section, in such a system, there may be non-linear cooperative phenomena - congestion on the high pressure areas of both the macro (in the transition from one vessel cross-section diameter to another) or at the micro level (within one section arising due to the interaction of blood cells and plasma proteins).
The bloodletting procedure widely practiced by our ancestors helped the regulation of blood flow and was found by an empirical practical actions without theoretical foundation, improving the patient's condition. At the present stage we consider bloodletting as appropriate, since it leads to a decrease in blood pressure. This procedure can take a blood sample through a sterile packaging for subsequent autologous transfusion (without additional checks on the group and rhesus compatibility, the risk of contracting many types of infections, blood-borne). This practice of drawing blood for autotransfusion is now widely practiced in Europe.
It is necessary to pay attention to another source of hypertension, it is difficult to be corrected only medication therapy aimed at changing blood pressure. This situation changes caliber arteries, where blood flows from the artery into smaller vessels until arterioles. The joints of these vessels due to the lack of elasticity of a slowing of blood flow, as a result of the reverse current flow of blood may twist to form clots and blood clots. With a significant build-up of blood pressure in large blood vessels (arteries) occurs, as noted by several researchers, a spasm of arterioles, until their paralysis in violation of the adjacent structures of the brain activity. Therefore, if you do not establish the blood flow in the arterioles, the treatment will be ineffective and will be long-term rehabilitation.
The above-described condition, we believe the second possible source of stroke (the first we consider venous stasis).
In the absence of a proper prevention of stroke, cerebral edema possible. Interstitial edema observed in the development of hydrocephalus and is characterized by an increase in the volume of the interstitial space, due to violations of the outflow of CSF. In this form of cerebral edema, brain cell function and blood-brain barrier is maintained.
Recently, when discussing the pathogenesis of brain edema, are increasingly focused on aquaporin type 4 - specialized channels are localized in astrocytes and responsible for the transport of water within cells and plays an important role in the correction of intracranial hypertension, which is one of the major intensive care objectives patients with acute stroke. It seems necessary for the treatment and rehabilitation of and apply before (for 200 years), magnesium sulfate therapy, the drug acting on the blood vessels and muscles of deducing them from spastic state. Additional arguments in favor of magnesium sulfate-Application are:
- Elimination arteriolospazma, improve microcirculation;
- Potentiation of the action of antihypertensive drugs;
- Increase production of prostacyclin by endothelial cells;
- Reduction in plasma renin activity;
- Decrease in the activity of angiotensin-converting enzyme;
- Reduction of platelet aggregation.
Blue blood - this is not a myth. The real, not artificial blood blue (as, indeed, blood and other colors and shades) occurs in nature, but not as a sign of aristocracy. Blue blood is found in many inhabitants of the seas: cephalopods, squid, cuttlefish, and other organisms. This blood, unlike red iron human hemoglobin has mednosoderzhaschim complex blue - keyhole.
Perftoran - a preparation for which there is no impermeable barriers, it is capable of delivering oxygen to ischemic sites, glucose. When the diagnosis of ischemic stroke his appointment shows up to take stock to the site of ischemia via mikroirrigatora.
In Europe today there is a broad research and application Perftoran type drugs. Unfortunately, our domestic developers of the drug died and Russia lost priority on their production. At the time, the drug was successfully tested in combat conditions. He was appointed in wounds to the head and a large blood loss. Stroke can also be attributed to such a serious condition.
When added to the treatment of drug perftoran Semax reduces the rehabilitation period, and increases the efficiency of the recovery of brain neurons. Semax has complex neuroprotection, whose main components are immunomodulation, inflammation inhibition of glial responses, improving maintenance of the trophic brain, inhibition of the synthesis of nitric oxide and oxidative stress reactions. The optimal daily dose Semax stroke of average weight is 12 mg (3 drops 1% solution in each nostril four times a day), with severe stroke 18 mg (3 drops 1% solution in each nostril 6 times a day).
Interesting experimental data on brain vessels, received IP Pavlov and his school in the 30th years of XX century. First of all, they found that the intracranial vessels are in a constant state of tonic contraction. In this regard are particularly compelling observation with an action on the tone of vascular intracranial carbon dioxide. It turned out that under the influence of excess carbon dioxide blood tone of intracranial vessels is sharply reduced, and for the elimination of the excess carbon dioxide degree of tonic contraction of vascular re-amplified and reaches the initial state.
Application carbogen (a mixture of carbon dioxide and oxygen 1: 1) via the anesthetic machine to the mixer used A.P.Nesterovym professor and his colleagues for spasmolysis retinal vessels and glaucoma and cerebral blood vessels, respectively. Therefore, we believe it is possible to use carbogen and in the treatment of stroke.
Condition of permanent tonic contraction of the vascular wall is peculiar, apparently, only the intracranial arteries, because intracranial veins characterized the thin-walled, and the almost complete absence in their muscle wall (Riese, 1935). Fluctuations in blood filling of intracranial veins and the regulation of blood outflow rate determined it is not so much the state of the tone of the venous wall, as the pressure of cerebrospinal fluid and pressure in the sinuses of the skull and extracranial venous system (where the blood was collected from the cranial sinuses). The mechanism of focal disorders intracranial circulation is a complete loss of tone, a paralytic condition of the walls of small blood vessels, caused by excessive accumulation of carbon dioxide in the pool spastic reduction artery.
In pathological cases, the reactivity of the intracranial arteries on their mechanical stretching and neurohumoral influence can be different in different arteries. This is the reason for the onset of focal changes in cerebral blood flow, which in hypertensive patients are quite common.
Excessive reaction of the vascular wall (a sharp reduction in its tonic) by one or other intracranial arteries occurs as a response to increased stretching her high blood pressure, ie, if there artery spasm, it inevitably comes into effect is another mechanism of pathologic changes in intracranial circulation. As practice shows, after the short-term anemization cerebral tone of intracranial vessels is significantly reduced. After a long anoxaemia the extent of this decline is very severe, and in fact in this case we can speak about the paralytic state of the vascular wall, coming as a result of anoxaemia.
Spasm of one or other intracranial arteries results in anoxaemia around the pool with the development of this artery is a paralytic condition of the vascular walls and the ensuing consequences in the form of first and foremost a violation of permeability of vascular wall in the area of their paralysis.
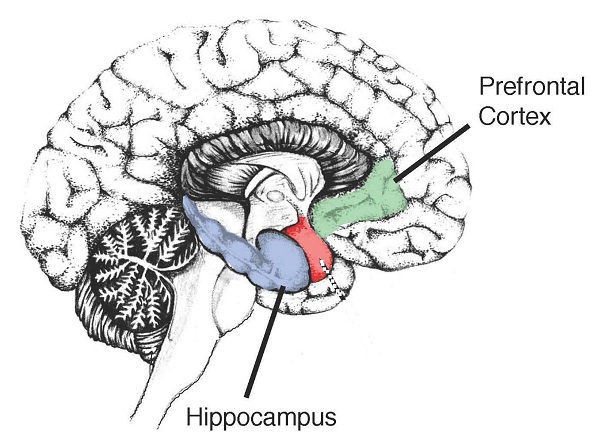
In the event of stroke it is also an important factor in the difference in electrical conductivity of certain brain structures. The experimental data of Pavlov and his students, intracranial elektropletizmografiya spread of electric current through intracranial formations indicates the possibility of following with utmost ease by cerebrospinal fluid, which, as it covers the brain fills the ventricles of the brain and has, as noted above, relatively high electrical conductivity . English researchers found that such pathology as epilepsy is the result of abnormal electrical discharge action in the brain cells.
However, liquor is not only through the distribution of electrical current within the skull. There is no reason to believe that the current should not be here on the brain tissue and the meninges. Due to the spread of current in intracranial vessels and there are pulse oscillation, which can be seen in each of intracranial electropletizmogramme.
Distribution of electric current through the cerebrospinal fluid is essential for the interpretation of the results of intracranial electropletizmography. The amount of liquor in the skull does not remain constant. On the one hand, the absolute amount may vary liquor (this apparently requires greater time intervals), on the other hand, it can be moved in different brain volume changes associated with variations in its blood supply or nerve tissue swelling.
In particular, it may be (L.V.Blumenau, 1889.) That liquor can be shifted to the tank of the medulla oblongata and the spinal subarachnoid space. If such transfers on the path of electric current inside the skull may be different amounts of liquor and thereby change the conditions of conduction of electric current in the cranial cavity.
Since living tissues possess the so-called ionic conductivity at passage through them of electric current latter meets some resistance, which can vary depending on several conditions: the mass of tissue in the path of the electric current changes its colloidal properties and richness of its first liquid medium containing dissolved electrolytes. Such environments should be classified: interstitial fluid, blood plasma, and applied to the study of the brain and spinal cord - and cerebrospinal fluid.
The highest electrical conductivity (least resistance) possess CSF and blood plasma. Good conductive muscle tissue, somewhat lower conductivity has nerve tissue and liver tissue. The relatively poor conductor of electric current is bone.
Wick and Alexander (1939) found that the conductivity of the blood column in the aorta decreases sharply when stopping circulation.
The relationship between blood flow rate and its electrical conductivity can be set at a constant and alternating electric current. These authors further showed that the faster moving blood, the more it increases the electrical conductivity. The difference in this case is quite considerable and may reach 15%.
Their data show that increasing the electrical conductivity and resistance drop of blood associated with its current acceleration; slowing blood flow leads to opposite changes in its electrical resistance.
In the experiment, and Alexander Wick also been shown that the lumen of intracranial arteries can be changed to some extent during stimulation of the cervical sympathetic and parasympathetic nerves. Furthermore, it was found that the tone of blood vessels and brain membranes significantly affects the chemical composition of blood and especially its content of carbon dioxide.
All of the facts of the blood and cerebrospinal fluid conductivity allow us to suggest the accumulation of brain cell electrical potential and its discharge in the brain tissue of stroke with a lesion of the structures in the form of burns.
In hemorrhagic stroke is a conflict of two genetically dissimilar systems: blood and neurons. It is known that neurons develop from the ectoderm as well as leather and match the female genotype, as develop from a part of the egg, unfertilized sperm. A blood, in turn, develops in the yolk sac, which is the result of fertilization by sperm polar body thus comprises the genetic material of both parents. Upon contact of the two systems is developing an autoimmune process, aggravating loss of brain tissue due to stroke. These studies on the genetic structure of cells in the brain and blood reported to us at the III Congress of Immunology and reproduction in Moscow and at the IV International Congress of Immunology and reproduction in Varna.
As you can see, the problem of stroke, considered by us as a disaster cerebral circulation, requires further study from different perspectives. For a visual representation of the biomechanics of the cardiovascular system and cerebral blood flow, in particular, it is an interesting simple analog electric model of a circulation system.
There is a paradoxical situation that is incomprehensible to the common man. There is a cure, that says that it is an analgesic, it takes a person who has a pain, but the pain persists.
It is very effective in neuropathic pain and anticonvulsants. This group of drugs has a rich history. Among the modern anticonvulsants have drugs that act in the brain to synapse on dorsal horn level, where the first neuron is joined with the second. This type of medication gabapentin (Neurontin) and pregabalin (Lyrica). The transmitter in the synapse, glutamate is the neuropathic pain and at the synapse works excessively. And Neurontin and Lyrics - are drugs acting through the calcium-mediated mechanism, blocking the chain reaction associated with the release of glutamate and its effect on the receptors, thus contributing to the reduction of glutamate activity and thus reduce the intensity of pain.
We are all familiar with the pain - whether it be the head, toothache or pain in the muscles after exercise. But there is quite a different pain that is associated with damage to the nerves. It is often a painful, violates a person's life over many months or years. This pain is called neuropathic. It occurs in 6-7 of 100 people. Neuropathic pain can make even the most basic actions, such as putting on socks, shirt, walk, impossible. Often people do not realize what kind of pain and how to tell your doctor about it. They can not find the words to describe it. So often, these patients do not receive proper care and treatment desired.
As there is neuropathic pain? In our body there are millions of nerves, interacting with each other. Together they form the nervous system. Imagine a set of electrical and telephone wires connecting your brain to various parts of the body. For example, when you step on the beach in the hot sand, nerves located on the foot, sending a signal to the brain that tells that you step on something hot. As a result, you feel in stop burning. Or, if you accidentally touch the exposed electrical wires, the nerves in the hand are sent to the brain faster signal that you electric shock. But if there is damage to the nerves, they begin to work properly and send incorrect signals to the brain. For example, the damaged nerves can inform the brain about the fact that you stepped on hot or touched the electric wires. And this despite the fact, that in fact you are nothing on advancing and not to touch anything. Nerves can be damaged as a result of many factors, such as diabetes, herpes infection, injuries of hands and feet, spine disorders, stroke, cancer and others.
Which diseases pain occurs after a stroke:
Characteristics of pain after stroke:
Approximately 8% of patients after cerebral stroke, after some time (from 1 month to 2 years) on the affected side, or in the arm and / or leg may appear unpleasant sensations as tingling, burning, pain on contact with cold objects, "hand is cold." Therefore, to reduce the pain after a stroke, some patients wear a mitten. This type of neuropathic pain is called post-stroke central pain. Its cause is damage to the nerves in the brain area.
Pain after a stroke or "central post stroke pain" - this pain and other sensory disturbances that occur after suffering a stroke. In 1906, Dejerine and Roussy described strong unbearable pain - thalamic syndrome (deep and superficial unilateral anesthesia, mild hemiplegia, sensory ataxia, choreoathetosis structurally unstable) after myocardial localized in the thalamus. A common cause of central pain - vascular lesion of the thalamus (ventroposteriolateralnyh and ventroposteriomedialnyh thalamic nuclei). Pain after stroke as well experience some at ekstratalamicheskih focal lesions (lesion of the lateral sections and the bridge of the medulla oblongata most common causes of these disorders - heart attacks, hemorrhage, arteriovenous malformations Pathogenesis of central pain in many ways remains unclear;.. Discuss the possible role of the defeat of afferent somatosensory systems in the brain, and also dizingibitsiyu, sensitization and secondary neurotransmitter disorders.
Epidemiology of pain after stroke.
Central post-stroke pain occurs throughout the year after suffering a stroke in 8% of patients. That is, the uptake of people with post-stroke pain great enough. 50% of patients affected by this pain syndrome during the first month after a stroke, 37% - in the period after the first month of the second year, and only 11% of patients after 2 years.
The clinical picture of pain after stroke.
Central post-stroke pain often occurs in the right or left side of the body, although some patients pain may be local (on the face in one arm or leg). Patients often describe the pain: burning, tingling, aching, tearing. Pain enhance various factors: cold, motion, heat, emotional outbursts. In other patients, these factors can reduce the intensity of pain. Such pain is often accompanied by other neurological symptoms: hypersensitivity, numbness, dysesthesia, changes in susceptibility to heat, cold, vibration and touch. A reliable diagnostic feature - abnormal sensitivity to cold and heat. According to studies, about 70% of patients with central post-stroke pain does not feel the difference in temperature between 0 and 50 ° C. Typical for these pains - the phenomenon of allodynia noted in 71% of patients.
In the treatment of post-stroke pain is the most efficient assignment of amitriptyline (75 mg / day or higher), with best results obtained at the first signs. Inefficient assignment of selective serotonin reuptake inhibitors, the same applies to carbamazepine. Do not give the effect of NSAIDs. The results of the use of opioid analgesics are also unsatisfactory because of the high incidence of side effects (although a number of studies and noted some positive effect). Taking into account the different pathogenetic mechanisms of pain after stroke is currently studying the effectiveness of a rational combination pharmacotherapy (antidepressants in combination with anticonvulsants and opioids).
The author of interviews with contemporary neuroscience professionals revealed that they have worked and are working on the basis of their plants remove spasticity and rigidity through the pain. It considered them a legitimate, binding and valid.
But in recent years the European school world neurologists unfolded toward analgesia in post-stroke period. For anesthesia during manipulations may also be used electroanalgesia. The equipment for this is widely and successfully used in the 20th century.
It is necessary to use anesthesia in neurology for the treatment of patients in rehabilitation period. It should be the emergence of a new medical specialty of anesthesiology and respective service. Neurologists, for unknown reasons, possibly because of their settings: treatment of spasticity through the pain, failed to notice the emergence of Anesthesiologists service and do not use it until now.
Conclusions:
1) pain relief in the domestic neurology is not enough developed;
2) is urgently needed staff unit anesthesiologist in stroke centers;
3) need rethinking of pain and its possible consequences, because during the manipulation of the affected organs arises "sews" the pain from head to toe. Pain, in our opinion - is an individual experience in sensation, feeling, nervous system response to changes in the operation (action) of an organism, an organ, or portion of the human body. This action of protective forces generated within the body and manifest themselves in the form of a sense of human consciousness. Pain - is a consequence of saying, the search for the cause. If the cause is identified, the pain must be eliminated, because in this case it is an obstacle to the treatment of disease.



 Cart
Cart