Anxiolytics
22 Dec 2016
Anxiolytics (from the Latin anxietas -. Anxiety, fear + Greek lytikos -. Capable of dissolving, weakening), or tranquilizers (from the Latin tranquillo -. Calm), or ataractics (from the Greek ataraxia -. Equanimity) - psychotropic drugs that reduce the severity of, or overwhelming anxiety, fear, anxiety, emotional stress.
Appearance of the first tranquilizers refers to the 50-th years of XX century. Prior to that, for the correction of anxiety use alcohol, opium, bromides (from the beginning of the XIX century.), Barbiturates (from the beginning of XX century.) And others. Means.
In 1952, during the search of the central muscle relaxant meprobamate was synthesized (meprotan). In 60-ies in a number of clinical trials were found anxiolytic properties (when taken in high doses - 100-400 mg / day) of hydroxyzine (Atarax) - one of the first antihistamines, an antagonist of H1-histamine receptors, is used in dermatology since 1955 The first generation of anxiolytics include also trimetozin (Trioxazine, repealed in 1996), the central anticholinergic benactyzine (Amizyl), atypical anxiolytics mebicar and Benzoclidine (Oxylidin).
Widely used in medical practice, drugs anxiolytics groups have since the 60s of XX century, when the first tranquilizers - benzodiazepine derivatives:. Chlordiazepoxide (Librium, 1960) and diazepam (Valium, 1962).
Historically, can be divided into 3 generations anxiolytics:
- The first generation of anxiolytics (meprobamate, hydroxyzine, benactyzine et al.);
- The second generation of anxiolytics (benzodiazepine drugs);
- The third generation of anxiolytics (buspirone, etc.).
There are several classifications of drugs belonging to the group of anxiolytics: chemical structure, mechanism of action, pharmacokinetic and pharmacodynamic characteristics and others.
According to the classification MD Mashkovskiy anxiolytics represented by several classes of chemical compounds:
- Benzodiazepines (benzodiazepines);
- Esters of substituted carbamic propanediol (meprobamate);
- Diphenylmethane derivatives (benactyzine, hydroxyzine);
- Tranquilizers different chemical groups (benzoklidin, buspirone, mebicar et al.).
- Benzodiazepine receptor agonists (diazepam, Phenazepam et al.);
- Serotonin receptor agonists (buspirone);
- Substances of various types of action (benactyzine et al.).
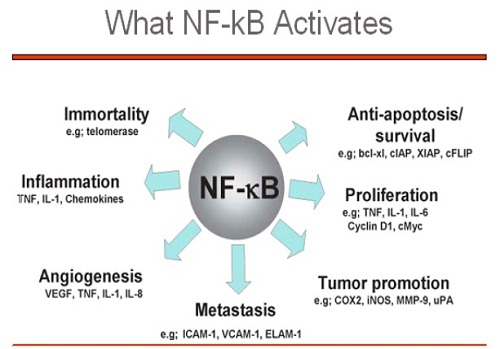
Mechanisms of action of anxiolytics has not yet been disclosed to the end. Action anxiolytics manifested by decreasing the excitability of the subcortical regions of the brain (the limbic system, thalamus, hypothalamus) responsible for the implementation of emotional reactions, inhibition of interaction of these structures with the cerebral cortex, as well as oppression polysynaptic spinal reflexes.
In the aspect of different neurochemical anxiolytics differ on the specifics of the action. The effect on noradrenergic, dopaminergic, serotonergic system is expressed in their relatively low degree (with the exception of buspirone). The effects of benzodiazepines are mediated effects on brain GABA-ergic system.
Currently leading position in wide use among drug group anxiolytic benzodiazepines continue to hold. Most structures benzodiazepine anxiolytics are 1,4-benzodiazepine derivatives. Basis benzodiazepine chemical structure consists of a benzene ring connected with the seven-membered heterocyclic ring containing two positions 1 and 4 nitrogen atom (diazepine) all used in the clinic benzodiazepine derivatives have also the second benzene ring attached to the carbon at position 5. For the manifestation of activity essential is the presence of a halogen or nitro group at the 7 position. Certain benzodiazepine compounds contain in the molecule the residue of 1,5-benzodiazepine (clobazam) or 2,3-benzodiazepine (Tofisopam).
Due to the easy replaceability radicals on different positions in the molecule benzodiazepine was synthesized and studied for more than 3 million compounds, of which a few dozen registered in different countries as drugs.
In accordance with the substituents in the diazepine ring benzodiazepines can be classified as follows:
- 2-keto-benzodiazepines containing keto-group at the carbon atom in position 2 (diazepam, dipotassium clorazepate, flurazepam * etc.);
- 3-hydroxy-benzodiazepines containing a hydroxy group at the carbon atom in position 3 (* oxazepam, lorazepam, temazepam *);
- Triazolobenzodiazepiny contain triazole ring connected to the diazepine ring through a nitrogen atom in the 1-position and the carbon atom in position 2 (alprazolam, triazolam * * estazolam).
Electrophysiological studies in the 60-70-ies. XX century., Showed that benzodiazepines enhance GABAergic transmission in the CNS. The mechanism of action of benzodiazepines was clear after in 1977, with the help of the method place radioligand specific binding of benzodiazepines was observed in the brain of humans and animals, so-called benzodiazepine receptors (receptors DB). Later on in vitro experiments and in vivo correlation was found between the ability of different benzodiazepines bind to these regions and their pharmacological activity. The methods of autoradiography and electron microscopy showed that the DB-receptors are localized mainly in the synapses of the CNS, primarily on postsynaptic membranes. It is shown that the heterogeneity of the DB-receptors, which are represented in the mammalian brain by at least two subtypes - BD1 and Sn2.
After detecting the specific binding sites of benzodiazepines began searching for endogenous compounds that interact with a DB-receptors, the so-called endogenous ligands. In a large number of compounds considered as the endogenous ligand-receptor DB: peptides, purines, nicotinamide hypoxanthine, beta-carbolines, diazepam binding inhibitor (DBI) and others, but the nature of the final database receptors endogenous ligand is not clear.
It is now believed that benzodiazepines interact with specific benzodiazepine receptors (agonists of these receptors), members of the postsynaptic GABAA receptor complex in the limbic system of the brain, the thalamus, the hypothalamus, the ascending activating reticular formation of the brain stem and neurons of lateral spinal cord horns. Benzodiazepines increase the sensitivity of GABA receptors to neurotransmitter (GABA) that causes the increase in the frequency of opening the channels in the plasma membrane of neurons to incoming currents chlorine ions. The result is a strengthening of the inhibitory effect of GABA interneurons and oppression transfer in the CNS.
he effect on GABA transmission - the main mechanism of action of benzodiazepine anxiolytics. A role in the implementation of the effects of benzodiazepine anxiolytics can play and other neurotransmitter systems of the brain.
Benzodiazepines have a wide range of pharmacological effects, including anxiolytic, sedative, hypnotic, muscle relaxant, anticonvulsant, amnestic and others.
The effects of benzodiazepines due to the influence on different parts of the central nervous system: amygdala limbic system (anxiolytic), the reticular formation of the brain stem and the nonspecific nuclei of the thalamus, the hypothalamus (a sedative and hypnotic), hippocampus (anticonvulsant).
The main effect, characteristic for all drugs combined into a group of anxiolytics, and makes use of these funds for all types of anxiety disorders, is an anxiolytic (anti-anxiety). The anxiolytic effect is a decrease in anxiety, fear (anti-phobic effect), emotional tension.
Sedative (calming) effect is a decrease in psychomotor excitability, daily activities, decreased concentration, decreased reaction rate, and others.
Hypnotics (hypnotic) effect is to facilitate sleep onset and increase its duration. The inhibitory effect of tranquilizers on the CNS contributes to strengthening the mutual effects of hypnotics, anesthetic and analgesic agents.
Muscle relaxant activity (relaxation of skeletal muscles) is due primarily to inhibition polysynaptic spinal reflexes. Benzodiazepines may also provide and direct depressant effect on motor nerves and muscles function. Myorelaxation effect of the application of tranquilizers is often a positive factor for stress relief, arousal, including motor, but it can also limit the use of drugs in patients who require rapid mental and physical reactions. Note that the muscle relaxant effects can manifest a sense of lethargy, weakness, and others.
The anticonvulsant effect is to suppress the spread of epileptogenic activity occurring in the epileptogenic foci in the cortex, the thalamus, and limbic structures. Anticonvulsant action is connected not only with the effects on the GABAA receptor complex, but also due to the effect on the voltage-gated sodium channels.
Amnestic effect (ability to induce amnesia) occurs mainly with parenteral use (diazepam, midazolam *, etc.). The mechanism of this effect is not yet clear.
The spectrum of action of some tranquilizers sometimes emit additional effects, including vegetative stabilization. Vegetative-stabilizing effect is due to the normalization of the functional activity of the autonomic nervous system. Clinically, this effect can be expressed by a decrease in autonomic manifestations of anxiety (unstable blood pressure, tachycardia, sweating, violation of gastrointestinal function, and others.). Expressed Wegetotropona action have Tofisopam, diazepam, etc. hidazepam.
Benzodiazepine derivatives may exhibit all the characteristics of this group pharmacological properties, however, and the severity of effects at different ratio of benzodiazepines may be different, which makes use of certain features of clinical drugs.
The peculiarities of the clinical actions of benzodiazepine anxiolytics can be divided into 3 groups:
1). Benzodiazepines with a predominance of anxiolytic action.
2). Benzodiazepines with a predominance of hypnotic action.
3). Benzodiazepines with a predominance of the anticonvulsant action.
Anxiolytic effects have Phenazepam (for anxiolytic activity surpasses many benzodiazepines, including diazepam), diazepam, lorazepam, alprazolam, and others. Moderately pronounced anxiolytic effects from chlordiazepoxide, bromazepam, gidazepam, Clobazam, oxazepam and others.
Sedative-hypnotic effect is particularly pronounced in nitrazepam * * flunitrazepam, flurazepam * * temazepam, triazolam * * midazolam, estazolama * et al. And they are used mainly as hypnotics (see. Hypnotics).
Anticonvulsant properties characteristic clonazepam, diazepam, and also (in lesser extent) for nitrazepam etc. *.
Muscle relaxant activity is characteristic of diazepam, chlordiazepoxide, lorazepam, tetrazepam and others.
For some anxiolytics characteristically pronounced anxiolytic effect at relatively low muscle relaxant and hypnotic (Tofisopam, medazepam et al.), In connection with which they are more convenient for use during the day (the so-called daytime tranquilizers).
Benzodiazepine derivatives differ in their pharmacokinetic characteristics, which is also taken into account in the appointment of these drugs. For the duration of action (taking into account the effect of the active metabolites), benzodiazepines can be classified as follows:
- Long-acting (T1 / 2 - 24-48 h): diazepam, chlordiazepoxide, etc .;
- Average duration (T1 / 2 - 6-24 h): alprazolam, oxazepam, lorazepam etc .;
- Short-acting (T1 / 2 - less than 6 hours): midazolam, etc. *.
When administered benzodiazepines are well absorbed from the gastrointestinal tract, mainly from the duodenum (absorption depends on several factors, including by lipophilicity). The most rapidly absorbed diazepam and triazolam *, the least fast - oxazepam, lorazepam. Antacids can decrease rate (but not the extent of absorption) some benzodiazepines, including chlordiazepoxide and diazepam. After intramuscular administration of benzodiazepines are absorbed more slowly than when taken orally (with the exception of lorazepam and midazolam *, which with the / m introduction absorbed quickly).
The time to reach maximum plasma concentration after a single dose for different drugs varies from 30 minutes to several hours. Equilibrium concentration in the blood at course intake of benzodiazepines is usually achieved within a few days after initiation of therapy (for benzodiazepines with short half-life and the mean) or within 5 days - 2 weeks (for drugs with long half-life). Benzodiazepines and their metabolites are characterized by a high degree of binding to blood proteins, ranging from 70% (alprazolam) to 98% (diazepam).
High lipophilicity results in penetration of the drug through the BBB and other biological barriers, as well as a significant rate of redistribution of CNS tissue (adipose tissue, muscle). The volume of distribution of benzodiazepines is quite high.
Benzodiazepines primary metabolism in the liver. Exceptions are dipotassium clorazepate and flurazepam *, which are rapidly metabolized in the gastrointestinal tract and enter the blood system in clinically relevant amounts. Action exert their active metabolites that subsequently undergo biotransformation in liver. Most benzodiazepines subjected to liver microsomal oxidation, mainly by N-demethylation and hydroxylation to active or inactive metabolites. Then metabolites undergo further conjugation or biotransformation. You can also like Phenibut.
In the metabolism of many benzodiazepines same active metabolites are formed, some of them are used as distinct drugs (oxazepam, etc.). The duration of the therapeutic effect of benzodiazepines having active metabolites determined not T1 / 2 of the starting material, and T1 / 2 of active metabolites. For example, T1 / 2 desmethyldiazepam (nordiazepam), which is an active metabolite of chlordiazepoxide, dipotassium clorazepate diazepam and is, according to one more of 30-100 hours, at the other - 40-200 hours, far exceeding half-lives of the starting materials.
Some benzodiazepines do not form active metabolites -. Lorazepam, oxazepam, temazepam *, etc., subject only under the influence of the process of conjugation to glucuroniltransferaze to form a glucuronid.
Benzodiazepines (and their metabolites) are derived primarily through the kidneys as conjugates, less than 2% - unchanged, a small part - through the intestines.
Some benzodiazepines pharmacokinetic parameters depend on age. For example, elderly patients may increase the volume of distribution. Furthermore, elderly patients and children may be extended half-life.
Time of occurrence and duration of the effects of benzodiazepine anxiolytics are not always related to their half-life, but the course intake, these parameters are largely correlated. When receiving repeated doses of the benzodiazepines with long T1 / 2 occurs accumulation of the drug and / or its active metabolites. A related effect is the aftereffect of drugs (diazepam, etc.). The accumulation of benzodiazepines with a short or medium half-life is usually minimal, and they are quickly eliminated from the body after the end of therapy.
The spectrum of anxiolytics clinical use due mainly to their anti-anxiety effect. Benzodiazepines are used in all types of anxiety disorders (which may be indicated for the treatment of anxiety disorders or for the short-term elimination of symptoms of anxiety).
In psychiatric and neurological practice anxiolytics are used in the treatment of neuroses, psychopathy states, accompanied by anxiety, fear, increased irritability, emotional stress. For relief of anxiety and phobic disorders (panic attacks, etc.) With the most effective drugs anxiolytic and anti-phobic effect - alprazolam, lorazepam, Phenazepam. Some benzodiazepine anxiolytics are used for the relief of anxiety syndrome at endogenous mental illness, including in schizophrenia (as an aid in the complex therapy) - diazepam, Phenazepamum and others.
In acute conditions, such as the purpose of the relief expressed psychomotor excitation, effectively parenteral administration of benzodiazepines (diazepam, Phenazepamum et al.).
When acute alcohol withdrawal anxiolytics (diazepam, Oxazepam, Phenazepamum, chlordiazepoxide, etc.) is used in the complex therapy to relieve symptoms such as excitement, nervousness, restlessness, anxiety, tremors, and also to reduce the probability of developing or signs, in Vol. h. hallucinations, emerged acute delirium.
When sleep disorders using benzodiazepines, have, along with anxiolytic, hypnotic action marked (* nitrazepam, flunitrazepam * * triazolam, temazepam * etc.). They relieve emotional stress, reduce anxiety, anxiety and promote sleep onset. Application of sleep disorders benzodiazepines such as diazepam or Phenazepamum advisable in cases when combined with insomnia and daytime anxiety desirable that anxiolytic effects lasted throughout the day.
Benzodiazepines with pronounced anticonvulsive action can be effective in the treatment of epilepsy, status epilepticus (clonazepam, diazepam, etc.), Nitrazepam * - in some forms of seizures, especially in children.
Benzodiazepines, like other anxiolytics, are widely used in many fields of medicine: cardiology, anesthesiology and surgery, dermatology and others.
Some benzodiazepines with marked muscle relaxant action (diazepam, chlordiazepoxide, and others.) Are shown in spastic conditions associated with damage to the brain or spinal cord, and others.
Benzodiazepines are used for sedation before and immediately before surgery and endoscopic procedures for induction of anesthesia, when ataralgezii combined with analgesics (flunitrazepam * * midazolam, diazepam, etc.).
The use of anxiolytics some healthy people may be justified for acute reactive states of stress in extreme situations (fire, industrial disaster, earthquake, etc.). Keep in mind that anxiety or tension associated with everyday stress, are not an indication for anxiolytics purpose, therefore should not be given them in any stressful conditions, particularly in reactions of grief or somatic diseases.
The main contraindications to the appointment of benzodiazepines is an individual hypersensitivity, severe liver failure, myasthenia gravis, glaucoma, severe respiratory failure, ataxia, suicidal tendencies, drug or alcohol dependence (except for the treatment of acute withdrawal syndrome).
Should avoid taking benzodiazepines during pregnancy (especially in I trimester) and lactation.
Benzodiazepines easily pass through the placenta. There is evidence that chlordiazepoxide and diazepam increase the risk of congenital malformations in the appointment in the I trimester of pregnancy. Other drugs in this group may also increase the risk, so the appointment of drugs benzodiazepine during pregnancy should be treated very carefully and use them only in the absence of alternatives, matching the potential risk to the fetus and the benefit to the mother.
In the appointment of benzodiazepines (clonazepam, diazepam and others.) During pregnancy, women with epilepsy should be aware that there are reports of increased incidence of birth defects in children whose mothers took anticonvulsant drugs during pregnancy, however, the causal link between the the facts have not yet been established. On the other hand, in women taking anticonvulsants (e.g., clonazepam), their cancellation before or during pregnancy is possible only in cases where seizures are weak and sparse in the absence of treatment, and if the probability of status epilepticus and withdrawal symptoms is evaluated as low.
The use of benzodiazepines in the III trimester of pregnancy (especially in the last week) can lead to accumulation of the drug in fetal tissues, and as a consequence, to the oppression of the central nervous system in newborns. This can be observed in the newborn muscle weakness, hypothermia, respiratory depression, disturbance of the sucking reflex.
Long-term use of benzodiazepines during pregnancy, including in late stages, it may lead to the formation of the development of physical dependence and withdrawal symptoms in the newborn.
The caution (only on strict conditions) used benzodiazepines during labor, for example, parenteral administration of diazepam in preterm labor or premature detachment of the placenta. Diazepam at low doses, usually has no adverse effects on the fetus, but the use of high doses can cause neonatal heart rhythm disturbances, decrease of pressure, asthma attacks, muscle weakness, etc. hypothermia. Symptoms.
Since benzodiazepines penetrate into breast milk in significant quantities, means that the group should not be applied to nursing mothers. Neonates benzodiazepines metabolized more slowly than adults, resulting in these drugs and their metabolites can accumulate in the body and cause sedation. It is possible feeding difficulties and weight loss in infants.
At therapeutic doses, benzodiazepines do not typically affect the function of respiration, blood pressure did not change. However, in patients with obstructive lung disease, a syndrome of sleep apnea, and others. While taking these drugs may worsen the condition.
Parenteral administration of benzodiazepines, especially in patients with middle and old age, can lead to breathing disorders (apnea) and the cardiovascular system (hypotension, bradycardia up to cardiac arrest).
Benzodiazepines not recommended as a single agent in the treatment of anxiety and depression or in severe depression because possible suicide attempts (benzodiazepines could enhance the expression of depression). However, some of the benzodiazepine anxiolytics structure (alprazolam, lorazepam, oxazepam) are effective in the treatment of anxiety depression on the background of various genesis (usually in combination with antidepressants).
Since most benzodiazepines biotransformation in the liver, in violation of its function may change the duration of the therapeutic effect of these drugs may cause serious side effects. In this connection it should be very careful when assigning benzodiazepines in patients with hepatic impairment.
The use of anxiolytics in children and adolescents under 18 years of age is justified only in exceptional cases, when well-founded indications, with the duration of treatment should be minimal.
Patients elderly, debilitated patients, children (especially small ones) are usually more sensitive to benzodiazepines neurotropic action. In particular to avoid systemic administration of benzodiazepines (especially a long acting) to patients over 65 years as intake of these drugs can lead to undesirable consequences in the form of excessive sedation, dizziness, disorientation and coordination. This may cause patients falls and related fractures.
Adverse side effects when taking benzodiazepines are signs of CNS depression, including daytime sleepiness, lethargy, muscle weakness, blunting of emotion, headache, dizziness, ataxia, and others. It is possible cognitive impairment (eg, chronic administration of diazepam, fenazepama).
In connection with a reduction in speed of psychomotor reactions, weakened concentration should be used with caution in outpatient anxiolytics, including Patients whose work requires quick mental and physical reactions, and is also associated with increased concentration (vehicle drivers and others.).
When receiving benzodiazepine anxiolytics possible paradoxical reactions (severe agitation, anxiety, hallucinations, nightmares, fits of rage, inappropriate behavior), most often seen in children, elderly patients and mentally ill patients. In the event of paradoxical reactions the drug should be discontinued immediately.
After receiving a few, mostly long-acting drugs (eg, diazepam), possible aftereffect syndrome (muscle weakness, decreased performance, and others.).
Application anxiolytics can lead to addiction (reduction effect of chronic administration) and the dosage form according to (physical and / or mental) and occurrence of withdrawal syndrome. The risk of dependence increases with prolonged use (more than 6 months), especially in high doses and in patients with alcohol dependence and drug history.
With a sharp lifting of the drug on a background of drug dependence may be withdrawal symptoms (tremor, convulsions, vomiting, excessive sweating), in severe cases - depersonalization, hallucinations, seizures (sudden elimination in epilepsy).
It should be remembered that treatment with anxiolytics can be conducted only under the supervision of a physician. In the appointment of benzodiazepines to treat anxiety disorders should respect the principle of gradual dose escalation - from the lowest to the optimum effective to produce a therapeutic effect (except for acute conditions). The course of treatment should be as short as possible, and then to re-evaluation of the patient to decide whether to continue therapy. Because of the possibility of addiction and the emergence of drug dependence WHO Conciliation Commission (1996) did not use the drug benzodiazepine continuously for more than 2-3 weeks. If necessary, long-term treatment (months) course should be done by the method of intermittent therapy, stopping the reception for a few days followed by the same dose of individually selected. The lifting should be done by gradual dose reduction, to reduce the risk of withdrawal symptoms.
In the treatment of anxiolytics should take into account the possible drug interactions of this group with other drugs. Anxiolytics potentiate the effects of other CNS depressants (opioids, anesthetic agents, hypnotics, antipsychotics with sedating, antihistamines to sedating effect), muscle relaxants, and others.
When receiving anxiolytics unacceptable consumption of alcoholic beverages, because alcohol increases the inhibitory effect of this group of drugs on the central nervous system (which may be accompanied by severe side effects, including loss of consciousness, respiratory depression), in turn, tranquilizers increase the toxic effect of alcohol on the central nervous system. In an application with alcohol in addition to increased inhibitory effect on the central nervous system are possible paradoxical reactions (psychomotor agitation, aggressive behavior, state of pathological intoxication).
Simultaneous administration of benzodiazepines with other drugs, oppressive central nervous system, as well as alcohol can lead to overdose and life-threatening consequences (in the case of serious overdose require medical intervention).
Symptoms of overdose may be anxiolytics oppression CNS varying degrees of symptoms (from somnolence to coma), including: expressed drowsiness, lethargy, weakness, loss of muscle tone, ataxia, in more severe cases - prolonged confusion, oppression reflexes, coma, and possible hypotension, respiratory depression. When intoxication benzodiazepines, induce vomiting, application of activated charcoal, gastric lavage through the probe (if the patient is unconscious), symptomatic therapy, requires monitoring of vital functions, in / in a liquid (to increase urine output), if necessary - the ventilator. Hemodialysis is an overdose of benzodiazepines is ineffective.
Specific benzodiazepine receptor antagonist is flumazenil - 1,4-benzodiazepine derivative with high affinity to benzodiazepine receptors. It competitively blocks the benzodiazepine receptors and eliminates or reduces the severity of the central effects of substances which excite these receptors, but does not preclude the action on the CNS with other means of depressing effect (barbiturates, opioids, etc.). The use of flumazenil as a specific antidote in overdose of benzodiazepines is possible only in conditions of a hospital. It should be borne in mind that the use of flumazenil as an additional, rather than as a single agent. The on / in the introduction of flumazenil acts quickly, but short-lived (the action of benzodiazepines lasts longer), so can be returned overdose symptoms. In addition, the possible development of epileptic seizures (especially in patients taking benzodiazepines, along with tricyclic antidepressants in patients with epilepsy).
Despite the fact that benzodiazepines has a leading position in the degree of knowledge and breadth of application, also other anxiolytics are used in medical practice.
So far, I have not lost their importance Benzoclidine. Benzoclidine reduces the activity of cortical neurons and inhibits the activity of the reticular formation of the brain stem, reduces the excitability of the vasomotor center, improves cerebral blood flow. It is used in the treatment of anxiety disorders, including anxiety-depressive states (especially mild expressed and associated with cerebrovascular insufficiency). Especially shows elderly patients with atherosclerosis with cerebral disorders, hypertension, paroxysmal tachycardia.
The return of interest to hydroxyzine due to the peculiarities of its pharmacological action. Hydroxyzine is an antagonist of the central m-choline and of H1-histamine receptors. Sedating and mild anxiolytic effect is due to inhibition of the activity of certain subcortical structures of the central nervous system. Hydroxyzine has quite rapid development of anxiolytic action (within the first week of treatment), the absence of amnestic effect. Unlike benzodiazepines, hydroxyzine long-term use does not cause addiction and dependence, withdrawal symptoms were observed, "return." In addition to use in the treatment of anxiety disorders, including psychosomatic diseases, it is used for sedation, relief of alcohol withdrawal syndrome, as well as itching dermatoses.
From other anxiolytics differs significantly benactyzine (diphenylmethane derivative), anxiolytic effect which is caused by reversible blockade of the central M-cholinergic receptors. Due to the pronounced influence of the central structure holino-reaktive benactyzine belong to the group of central anticholinergics. His influence on the central nervous system manifests sedative effect, inhibition of convulsive and toxic effect of cholinesterase and cholinomimetic substances, increasing the action of barbiturates and others. Hypnotics, analgesics and others. At present, due to the presence of effective tranquilizers, as well as due to the undesirable side effects, atropine-related effects (dry mouth, tachycardia, mydriasis, etc.), benactyzine practically applied as anxiolytic.
Propanediol derivative (meprobamate) effect on benzodiazepine and cholinergic receptors has not. Its anxiolytic effects due to the depressing effect on the various departments of the central nervous system, including the thalamus and the limbic system, muscle relaxant effect is due to inhibition of the transfer of excitation in the neurons of the spinal cord lateral horn, thalamus and hypothalamus. Besides the treatment of anxiety disorders, meprobamate used for menopause and premenstrual syndrome. It is less effective than the benzodiazepines, and currently has a limited application.
The third generation of anxiolytics are buspirone, hydroxymethyl-ethylpyridine succinate (Mexidol) and others. Mexidol anxiolytic effect is due to its modulating effect on the membrane, including GABAA receptor complex, and shows improvement in synaptic transmission.
The mechanism of action of buspirone is not completely understood. Buspirone is a partial agonist of the serotonin receptor has high affinity for the serotonin receptor subtype 5-HT1A. Decreases the synthesis and release of serotonin, the activity of serotonergic neurons, including in the dorsal raphe nucleus. In addition, it selectively blocking (antagonist) pre- and postsynaptic dopamine D2-receptors (having moderate affinity) and increases the rate of excitation of the midbrain dopamine neurons. Some evidence about the presence of buspirone effects on other neurotransmitter systems. Buspirone is effective in the treatment of mixed anxiety-depressive states, panic disorders, and others. Anxiolytic effect develops gradually, seen in 7-14 days, and reaches a maximum after 4 weeks. In contrast to benzodiazepines, buspirone no sedative action, adverse effects on psychomotor functions, does not cause tolerance, dependence and drug withdrawal symptoms, do not potentiate the effects of alcohol.
In addition to drugs belonging to the group of anxiolytics, in varying degrees, have anxiolytic action of pharmacological agents of other groups, some beta-blockers (propranolol, oxprenolol, acebutolol, timolol et al.), Alpha-adrenoceptor agonists (clonidine). Thus, propranolol is effective in the treatment of anxiety states associated with hyperactivity of the sympathetic nervous system and is accompanied by considerable severity of somatic and autonomic symptoms, clonidine has the ability to reduce the somatic-vegetative symptoms with withdrawal syndrome opioid addiction.
In the treatment of anxiety disorders, including under compulsion, panic disorders, showing some antidepressants. In severe anxiety disorders pronounced effect gives some drugs from the group of neuroleptics.
There is an ongoing intensive search for new drugs with anxiolytic effects and at the same time safer and more effective than existing drugs. Screening benzodiazepine derivatives aimed at identifying more selectively acting drugs with the most pronounced anxiolytic effect with minimum side effects. Search also held among the substances that affect serotonergic transmission, antagonists of excitatory amino acids (glutamate, aspartate) and others.

 Cart
Cart