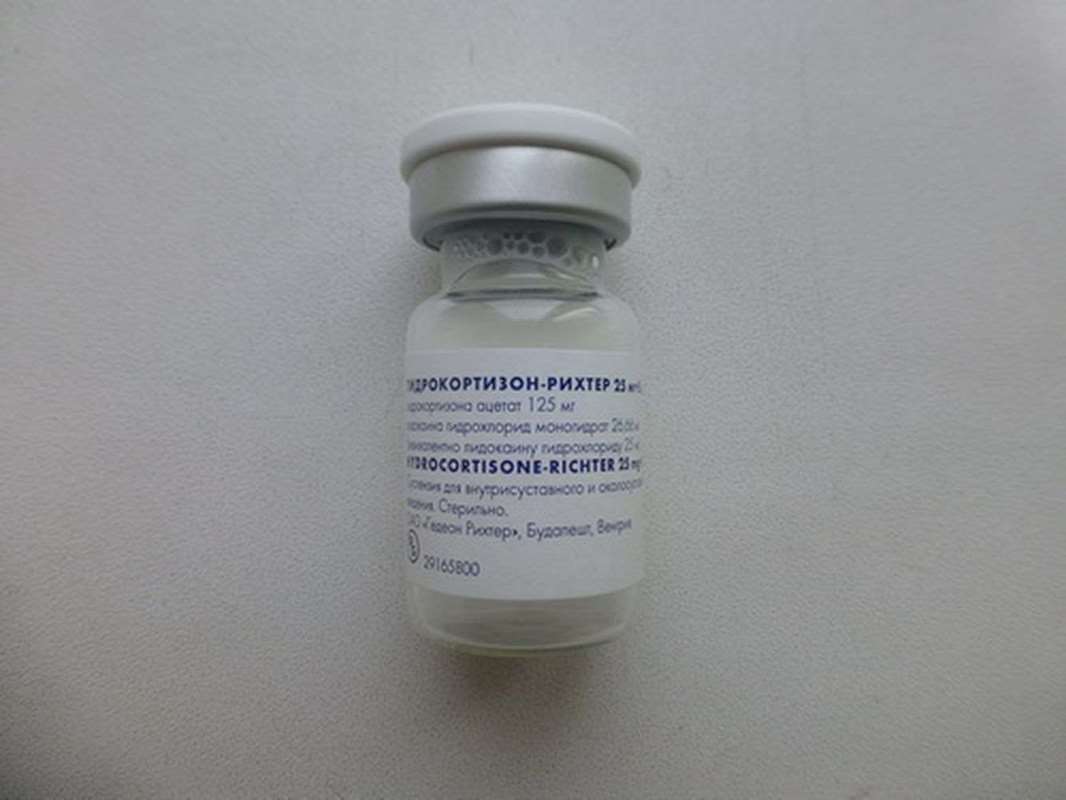
Hydrocortisone-Richter - glucocorticosteroid agent, anti-inflammatory effect.
Pharmacological properties
Pharmacodynamics: Hydrocortisone Acetate - glucocorticosteroid agent. Anti-inflammatory effect. Hydrocortisone inhibits the release of cytokines (interleukins and interferon) from lymphocytes and macrophages, eosinophils inhibits the release of inflammatory mediators, reduces the intensity of arachidonic acid metabolism and prostaglandin synthesis. Activates steroid receptors induces lipokortinov having antiedematous activity. It reduces inflammatory cell infiltration, prevents the migration of leukocytes and lymphocytes to sites of inflammation. In high doses, it inhibits the development of lymphoid and connective tissue. By reducing the number of mast cells, reduces the formation of hyaluronic acid; It inhibits hyaluronidase, thereby reducing capillary permeability. It is intended for intramuscular, intra- and periarticular administration to provide systemic or topical anti-inflammatory activity. With intraarticular injection therapeutic effect occurs within 6-24 hours and last for several days or weeks.
Lidocaine - local anesthetic with membrane-stabilizing effect in the short term has analgesic effect.
Pharmacokinetics:
When intra-articular and periarticular administration of hydrocortisone penetrates into the systemic circulation. Communication with the proteins - more than 90%. It is metabolized in the liver and tetragidrokortizon tetrahydrocortisol that the kidneys in a conjugated form. It penetrates through the placental barrier.
Lidocaine is well absorbed, it has a high affinity to plasma proteins.
It is metabolized primarily in the liver. The half-life - 1-2 hours.
Lidocaine passes into breast milk, placental and blood-brain barriers.
Inducations:
- Rheumatic diseases accompanied by arthritis, including osteoarthritis in the presence of synovitis (except for tuberculosis, gonorrhea, purulent and other infectious arthritis);
- rheumatoid arthritis;
- Frozen shoulder;
- Bursitis;
- Epicondylitis;
- Tenosynovitis.
Drug interactions:
- In Addison's disease co-administration with barbiturates can cause a crisis. It increases the toxicity of cardiac glycosides (proaritmogennoe act hypokalemia).
- Decreases hypotensive effect of antihypertensive drugs. Accelerating the elimination of acetylsalicylic acid, reducing its concentration in the blood.
- If you cancel the hydrocortisone concentration of salicylates in the blood may increase and lead to the development of adverse reactions. Both drugs have ulcerative effect, the simultaneous use of them can increase the risk of ulceration and bleeding.
- Vaccination live virus vaccines and conduct immunization of other species during treatment with hydrocortisone promotes activation of viruses and the development of infections.
- Increases isoniazid metabolism, mexiletine, especially in patients - fast acetylators, lowering plasma concentrations of these medicinal products.
- It enhances the hepatotoxic effects of paracetamol, since induces liver enzymes and the formation of toxic metabolites of paracetamol.
- Long-term treatment increases the content of folic acid.
- Hypokalemia caused by SCS, increases the severity and duration of muscle blockade of muscle relaxants.
- High doses of hydrocortisone reduces the effect of growth hormone.
- Reduces the effectiveness of oral hypoglycemic agents may require dose adjustment.
- It reduces or enhances the effect of anticoagulant drugs.
- Ergocalciferol and parathyroid hormone hinder the development of glucocorticosteroid osteopathy.
- It reduces the concentration of praziquantel in blood.
- Cyclosporine inhibits the metabolism of hydrocortisone.
- Ketoconazole decreases clearance and increases the toxicity of hydrocortisone.
- Thiazide diuretics, carbonic anhydrase inhibitors, amphotericin B, theophylline and other corticosteroids increase the risk of hypokalemia.
- Sodium-containing medicines contribute to the formation of edema and increased blood pressure.
- NSAIDs and ethanol contribute to ulceration of the mucous membrane gastrointestinal bleeding and Development. Hydrocortisone in the treatment of arthritis in combination with NSAIDs should be to reduce the dose of hydrocortisone to avoid additive therapeutic effect.
- Indomethacin, displacing hydrocortisone from its association with proteins, contributes to the development of adverse reactions of the latter.
- Amphotericin B and carbonic anhydrase inhibitors increase the risk of osteoporosis.
- Phenytoin, barbiturates, ephedrine, theophylline, phenylbutazone, rifampicin and other inducers of microsomal liver enzymes decrease the effects of hydrocortisone, increasing its metabolism.
- With simultaneous use of mitotane and other inhibitors of the adrenal cortex may be necessary to increase the dose of hydrocortisone.
- Drugs - Thyroid hormones increase the clearance of hydrocortisone.
- Immunosuppressive agents increase the risk of developing infections, lymphoma and lymphoproliferative processes caused by Epstein-Barr virus.
- Estrogens, including oral contraceptives estrogenosoderzhaschie reduce hydrocortisone clearance, extending the half-life and enhancing therapeutic and toxic effects of the latter.
- Concomitant use with other steroid hormone drugs (androgens, estrogens, anabolics, oral contraceptives) contributes to the development of acne and hirsutism.
- Not recommended for tricyclic antidepressants to treat depression caused by hydrocortisone, because they can worsen the course of depression.
- Simultaneous treatment with M-holinoblokatorami, including antihistamines, tricyclic antidepressants and nitrates promotes intraocular pressure.
- Action GCS weakened when taken with mifepristone.
Contraindications:
Hypersensitivity to any component of the drug; the infected joint; Cushing's syndrome; the tendency to thrombosis; I trimester of pregnancy; systemic infection without specific treatment; diseases of the Achilles tendon.
Intra-articular administration is contraindicated when undergoing arthroplasty, abnormal bleeding (endogenous or caused by anticoagulants), intra-articular fracture of the bone, infectious (septic) arthritis and periarticular infections (including history), general infectious disease marked periarticular osteoporosis, osteoarthritis without synovitis (so called "dry" joints), joint laxity, aseptic necrosis of the formative joint epiphyses of bones, severe bone destruction and deformation of the joint (a significant narrowing of the joint space, ankylosis).
Suggested Use:
Intra- and periarticular. One day Hydrocortisone-Richter may be administered no more than 3 of the joint. Repeated injection is subject to the 3-week interval. Introduction Hydrocortisone Richter directly into the joint may have an adverse effect on the hyaline cartilage, so the same joint can be treated with no more than 3 times a year.
If tendinitis injection should be done in the vagina tendon - directly into the tendon can not enter.
Adults: depending on the size and severity of the joint disease 5-50 mg intra- and periarticular.
Children: 5-30 mg / day, divided into several doses. A single dose of periarticular administration to children aged from 3 months. up to 1 year: 25 mg; from 1 to 6 years: 25-50 mg; from 6 to 14 years: 50-75 mg.
Packaging:
- Comes in original packaging. Item is brand new and unopened.
Storage:
- Keep away from direct sunlight.
- Keep locked and away from children.
- Store in dry place at room temperature.
- Do not exceed storage temperature higher than 30 C
Important notice- the outer box design may vary before prior notice!

 Cart
Cart