04 Nov 2016
About the impact of postpartum depression on the mother and child and the different approaches to its treatment.
The review article deals with the problem of postpartum depression (postpartum depression, PPD). As is known, the state of PPD is fraught with a number of serious consequences for the woman and for the child; It can lead to lag deviations in its physical, mental and emotional development.

The authors used clinical data and results of own experimental studies on animals, which allows a better understanding of the nature and causes of PPD. The article described the occurrence and the main symptoms of postpartum depression; analyzed the most important biological and social risk factors for this disease.
Also in the survey provides information on the currently available diagnostic methods and treatment of PPD. A significant part of the article is devoted to the description of model of postpartum depression in laboratory animals. They specially treated neuro-anatomical, endocrine and neurotransmitter bases maternal motivation in health and disorders of the nervous system.
The final section presents a group of drugs, promising in terms of features specific correction of post-natal depression.
Prevalence and Symptoms
Parent or postnatal depression (postpartum depression, PPD) is isolated from the group of depressive disorders of the psyche as a separate disease mainly by time criterion - pathology develops in the period of up to one year after birth. According to data obtained in the different studies, such a state is registered in 10-15% of women, and are sometimes referred wider occurrence limits. In many cases, PPD is a continuation of disorders, initially available to the women, as well as occurring during pregnancy, but further we will consider features of maternal depression that occurs just after birth.
The high frequency of PPD in the population contrary to popular belief about childbirth as a panacea for mood disorders and mental disorders. In addition, the depression-like symptoms in the perinatal period often seen a young mother and her surroundings as an insignificant phenomenon, which itself will take place later. With these and some other reasons linked to a weak level of knowledge of maternal depression, particularly in countries with a lower standard of living. People often do not realize the need of medical care in this situation.
Young mother spent a huge force on child care, often almost do not care about their own mental state. With the development of depression, it is fraught with eating disorders, lack of attention to health regulations on care and newborn. It has been shown that women who suffer from postpartum depression, often inadequately assess their own emotional reactions of the child, especially the negative ones.
In addition, the main symptoms of PPD include:
- -constant fatigue, sleep disturbance and appetite;
- -a state of deep sadness and emptiness, "emotional stupidity"; frequent crying;
- -exclusion from family, friends, previously enjoyable activities;
- -great concern and worry about the baby, fear of harm to him or, conversely, lack of interest in the newborn;
- -thoughts of suicide.
This condition is often accompanied by increasing consumption of tobacco, alcohol and drugs, as well as an extremely negative impact on the atmosphere in the family.
The impact on the mother and child
In addition to the violation of women's mental health, postpartum depression can lead to certain physical disorders, such as frequent headaches, disruption of the menstrual cycle. The disease may be accompanied by other somatic symptoms: dizziness, nausea, chills, and the like. Along with mood disorder and general moral well-being of these symptoms have a significant impact on a woman's quality of life and increase the risk of health problems more serious in the future.
An extremely important consequence of maternal depression is that a violation of the interaction between mother and child can lead to deviations of the lag in its physical, mental and emotional development. It was found that maternal depression is a risk factor for psychopathology of offspring - in particular, depression, disorders of attention, increased excitability. The authors of studies conducted in experimental animals, this effect is associated with impaired development of the hypothalamic-pituitary-adrenal axis by tissue-specific effects on gene expression.
There Communications PPD data with reduced amounts of Apgar score and sleep disturbance in children aged 12 months and lower values IQ at age 14-15 years.
However, long-term studies of the dyad «mother in the doldrums ⇔ child» are not so much, and their results differ. For example, scientists studying the relationship of depression in the mother and the child's development up to two years according to the European clinics, showed no significant effect of PPD on body weight and other anthropometric indicators. The authors suggest that the correlation of these features in the works of other authors associated with research in countries with a low standard of living, where the presence of maternal depression is a component of a broader set of adverse effects. But in any case it is clear that a competent mother illness therapy will have a beneficial impact on child development.
Risk factors
Apart from having episodes of depression or other psychiatric disorders, a history of studies have identified risk groups with a high incidence of PPD. These include teenage mothers, single mothers, unemployed women, cases of unplanned pregnancy or severe its course, eating disorders. Elevated levels of stress during pregnancy, violence in the family also has a negative impact on the psychological state of the young mother.
In addition, the role played by children in the family, social support and relationships with friends and relatives, especially the nature of the relationship with the father of the child; significant influence presence of nicotine or other dependence. Even in developed countries postpartum depression often diagnosed in immigrant women (Canada). Some connections severity of PPD with the terms of the mother's work: security maternity leave, the ability to vary the employment schedule depending on the mode of child care and so on. Factors provoking the PPD, include the physical condition of women after childbirth: the presence of joints, fatigue, difficulty with toilet, eating, lack of comfort in the room. Young mothers who are afraid of losing the subtlety of the waist, are worried about the state of the figure, are sensitive to the appearance of sagging stomach, worry that they will not be able to restore the old form. It is shown that the formation of postpartum depression can affect the availability of excess weight during pregnancy. In addition, there is a change of social roles, interests and previous sessions sidelined, giving way to the role of homemaker and implementing parental motivation. Often the woman is in the postpartum period in a state of a kind of social and informational isolation, since the bulk of the effort and time needed to devote to the newborn. It is obvious that the direct participation and support of loved ones can ease her condition and prevent or ease the development of PPD.
In some studies, the authors trace the relationship the risk of postpartum depression with diet women - for example, intake of sufficient amounts of polyunsaturated fatty acids omega-3 or seafood. Most likely, these factors should be considered as part of a broader set of conditions. It is known that a varied diet full beneficial effect on pregnancy in general, and, therefore, a woman does not appear more cause for concern.
Neurobiology maternal motivation in normal
It is obvious that the search for effective treatments for postpartum depression and disorders of parental behavior is necessary to have an understanding of the specific mechanisms of formation of maternal motivation.
Based on laboratory studies in the past decade, we can conclude that for the different components of responsible parental behavior different areas of the central nervous system. However, they are all interlinked and form an integrated system that provides flexible control and regulation of the behavior of nursing mothers.
During the initiation and maintenance of maternal behavior in rats responsible primarily the medial preoptic area of the hypothalamus and the nucleus accumbens transparent partitions (nucleus accumbens, refers to the basal ganglia of the cerebral hemispheres). Numan The review indicated that the medial preoptic area of the hypothalamus, together with the location next to her bed nucleus of stria terminalis (BNST) facilitates the response of females to stimuli coming from the newborn. This occurs against the backdrop of evolved during pregnancy, immediately after childbirth and breast hormones (prolactin, estradiol, oxytocin). An important role of the medial preoptic area of the hypothalamus and BNST data confirm that their destruction leads to the complete or partial inhibition of maternal reactions.
Apparently, the described region of the brain not only activate specific maternal behavior, but also inhibit the amygdala and about mediated plumbing gray matter competing motivational state causing avoidance pups during pregnancy (backlash odor infants).
Numan et al. We have shown that the medial preoptic area of the hypothalamus sends glutamatergic efferents to such a structure, as the ventral tegmental area (VTA). VTA dopaminergic projections are, in turn, to an adjacent nucleus (NAcc). The nucleus accumbens in the ventral pallidum is projected (VP), associated with the front nuclei of the thalamus. The thalamus together with the frontal cortex provides a link between maternal motivation and movement, triggering the immediate implementation of behavioral programs.
Neurobiology PPD: hormone abstinence
Some studies suggest that postpartum depression observed in changes in the functioning of the neurotransmitter systems of the brain are partly the result of a sharp decline in the concentration of female sex hormones in the blood immediately after birth. To test this hypothesis, female rats chronically injected progesterone and estradiol, that mimicked hormones during pregnancy. After drug withdrawal growth was detected depressive manifestations in the experimental group compared to the control, while the indices of anxiety and general motor activity of rats did not differ. Another study showed that after the abortion on the 15th day of maternal behavior in female rats occurred after two or three days after the presentation of donor offspring. In the case of prior administration of estradiol parental reactions manifested immediately.
It is known that estrogen and progesterone are produced in large quantities during pregnancy and have extremely important for the maintenance of pregnancy and ensure timely delivery of successful peripheral influence. In addition, during pregnancy they seriously affect the brain by regulating the activity of various neurotransmitter systems and nerve centers, including the medial preoptic area of the hypothalamus.
Neurobiology PPD: congenital predisposition to depression
To investigate the mechanisms of depression manifestations used pharmacological agents or animal line with certain disorders of behavior. The second way allows you to identify the role of genetic susceptibility to maternal depression and PPD connection with certain hereditary diseases. For example, evidence of a general depression in rats WAG / Rij line, for which, moreover, is characterized by bouts of absence epilepsy. An increasing immobilization time during the "forced swimming" (reaction of "despair") and the decrease in the consumption of sucrose (anhedonia). The behavior of rats WAG / Rij corresponds to the symptoms of dopamine-dependent depression caused by receptors of the D2.
We have studied the maternal motivation in females of this line compared with females Wistar. It turned out that WAG / Rij rats are characterized by low intensity of parental reactions: the number of approaches to the newborn and the number of transfers was significantly reduced compared to Wistar. The cause of these and other behavioral characteristics inherent in WAG / Rij animals line, apparently, is a total disruption of the need-motivational centers of the brain associated with epileptiform stable status of the nervous system. We tend to treat the rats of the WAG / Rij as a genetic model of postpartum depression, which can be used to practice the methods of correction PPD.
Another example of such an approach are innately predisposed to depression rats Flinders Sensitive (FSL). Lavi-Avnon et al. It showed that the animals of this line, in contrast to the control (rats Sprague-Dawley), did not increase the amount of dopamine in the NAcc during contact with newborns. The intensity of the destruction of dopamine to the L-DOPAS have been higher. Rats Sprague-Dawley normally reacts as place preference, and they are of two identical cameras, unlike the FSL, choose one that is associated with cubs. It is interesting to know what other reinforcers (eg, after a period of drinking water deprivation) caused in FSL normal formation of preferences.
Neurobiology of PPD: the role of stress
The complex postpartum depression prevalence studies repeatedly show the effect of heavy stress situations during and after pregnancy on the risk of developing the disease. For example, more than 10% increased rate of depression in women exposed to "Katrina" hurricane, passed by the US southeast in August 2005. Have shown an increased risk of maternal depression in women, one way or another affected by the events of 11 September 2001 in New York. Among the stress factors affecting the development of the PPD, called the death of a loved one, divorce, job loss. Samu pregnancy and childbirth can be regarded as a state of physical and psychological stress for women, especially in the case of any complications.
At the level of stress of the nervous system accompanied by increased activity of the noradrenergic system. Its effects are able to compete with the action of dopamine, reducing maternal behavior. The literature suggests that there noradrenergic inputs, regulating the release of dopamine; It demonstrated that administration of noradrenaline in the VTA reduces the activity of dopaminergic neurons.
However, short-term (situational) stress can increase maternal behavior and in particular maternal aggression. In studies conducted in our laboratory, rats parental reactions are evaluated in different conditions - during the red (more comfortable) and bright (more stressful) illumination of the arena of the experimental setup. Observations show that the maternal behavior of females in bright light is activated. In this case, obviously, still manifests itself formulated AA Ukhtomsky dominant principle in a situation where the behavior is subject to predominantly maternal motivation, any additional unscathed sensory stimuli (eg, light) is capable of even more strengthen its manifestation.
Neurobiology PPD: pharmacological studies
The above described structure of the brain involved in the formation of both the maternal behavior and condition of postpartum depression. Operation of the corresponding neurotransmitter systems, particularly dopaminergic, changes not only at PPD development, but also when receiving neuroleptics - dopamine receptor antagonists.
It is shown that the damage or VTA administration NAcc dopamine antagonists leads to disturbances of maternal motivation. As a result, antipsychotics interrupt transition from parental motivation to appropriate behavior.
We found a negative effect of selective D1 blockers (SCH23390) and D2 (cleboprid) receptors in the maternal behavior of rats - females are smaller and slowly approached the young and transferred. Similar results were obtained when using the D2 - antagonist raclopride, which significantly reduced the number of shifts rats, but not the length of the female breast. Giordano et al. demonstrated that non-selective dopamine antagonist haloperidol when administered to lactating females dose-dependent manner violates transfers pups and building nests, but does not affect the intensity and duration of licking feeding. This same effect of haloperidol on the transfers described young Stern and Keer.
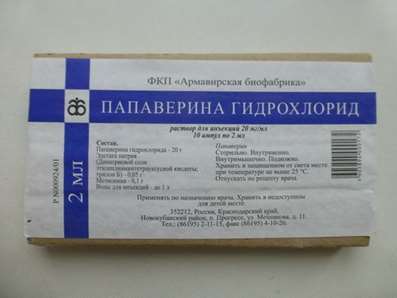
In animal experiments, atypical antipsychotics (mainly high-affinity 5-HT2A antagonists and low-affinity D2) showed a negative effect on the number of approaches to the young. Thus, the medium-dose effects of clozapine, risperidone, quetiapine, and became significant after half an hour after the use of drugs; inhibition of maternal behavior lasted about 4 hours. As well Phenibut, Phenazepam, afobazol can be used.
Very significant impact on the parent reaction provides the brain opioid system. The emergence of maternal behavior is closely associated with a decrease in its activity in the MPO. Injections of morphine in this area lead to a breach of manifestation of parental care during lactation. Another critical region involved in opioidergic blockade of maternal behavior is the periaqueductal gray (SALT). Introduction morphine SALT led to disruption of maternal behavior, the effect of the drug treated naloxone. The peptide agonists of opioid receptors (beta-endorphin, beta-casomorphins) also disrupt maternal behavior of white rats.
One of the modulators opioidergic regulation of maternal motivation is cholecystokinin. The blockade of its receptors enhances morphine induced violations of parental reactions. We consider this neuropeptide (and derivatives thereof) as pharmacological agents, potentially able to adjust the PPD. There is currently a similar assumption concerning the time and other peptide drugs - modulators behavior (e.g., ACTH fragments and analogues, vasopressin).
Chronic administration of lactating females drugs that impair maternal reaction is used to simulate the state of post-natal depression. Thus there is a long-term, stable malfunction of the neurotransmitter systems, for which the impact is. In the next step, the models are used to search for possible ways of PPD selective correction. They also make it possible to assess the likely breach the mother-child relationship with the regular intake of psychotropic drugs and drug compounds.
Path of correction PPD
An important feature of postpartum depression from the standpoint of therapy is that a significant number of cases lactating woman. Accordingly, when PPD drug medication with milk is transferred to the child. It has long been demonstrated that haloperidol, administered mother reaches the infant. Before the drug at a dose of 5 mg twice a day, its concentration in the mother's blood was 40 g / L in the milk - to 23 g / l. Thus, in this situation, a search of selective pharmacological ways to treat postpartum depression, has minimal effect on the child, as well as the development of non-drug treatment options.
When a weak depression severity is no doubt a positive effect of psychotherapy; also crucial support from the family and especially the wife. The literature describes a curious way to care for premature babies, are actively applied in the developing countries (Colombia, Nigeria), - Kangaroo Mother Care (KMC). The method is based on long closely baby and mother, a woman with a special fastening system carries a child on his chest under his clothes. Thus, on the one hand, significantly improved indicators of emotional and physical development of the newborn, the other - activated parental reaction.
In any variant of the disease is extremely important early diagnosis of PPD. To do this most commonly used scale of Edinburgh (Edinburgh Postpartum Depression Scale, EPDS) - a test that takes a little time and convenient for repeated measures. It includes 10 questions related to mood and well being of women in the last 7 days (can choose one of four options). The total score is calculated based on the severity of different types of moods and emotions (joy, sadness, despair, self accusation, suicidal thoughts, and others.). In some cases, women poll conducted by phone or mail, which greatly facilitates the diagnostic process for both the physician and for the mother. Less frequently used screening postpartum depression scale (Postpartum Depression Scrinning Scale, PDSS). However, many researchers believe it more appropriate than the EPDS, because 35 points PDSS questionnaire included questions assessing not just a state of depression, and depression in the context of the relationship of a woman with a child. The predictive accuracy of the PDSS is 94%, for the EPDS, the figure is 85%
Modern drug therapy PPD is primarily directed to modulation of the activity of dopaminergic and serotonergic systems in the brain directly by antidepressants. The most commonly used drugs for which there is no clinical evidence of adverse effects on child development with continued breastfeeding (Category B classification FDA - Food and Drug Administration, USA), such as bupropion. The drugs, which would be reliably shown no adverse effects on the offspring (category A), yet. It is obvious that such a specific pathology as postpartum depression, requires the development of special methods of medical correction, take into account the peculiarities of the physiological state of patients.
Other pharmacological approaches to the treatment of PPD
At the moment, we have already found several groups of compounds, looking from the point of view of the selective correction of post-natal depression.
For example, Wieck and his colleagues have confirmed the feasibility of PPD treatment with the dopamine agonist apomorphine receptor, which is administered at a dose of 0.005 mg / kg four days after birth. As a result of such therapy appears to increase the concentration of dopamine receptors, which positively affects the health of the patient. However, in order to reasonably provide apomorphine for use in clinical postpartum depression, it is necessary to carry out further detailed studies of its side effects on the mother and child.
On the basis of a possible role in the development of PPD postpartum hormonal withdrawal, some authors compared the nature of maternal depression with depression during menopause, which occurs due to lower production of estradiol. Subcutaneous injections of estradiol can help to cope with these conditions, but at the moment has not yet carried out the relevant gynecological studies testing the effect of the penetration of estradiol in milk, as well as security checks long-term administration of estrogen.
Our studies have found a positive effect on the motivation of the mother rats antagonist naloxone opioid receptors. It is shown that intraperitoneal administration of the drug at a dose of 5 mg / kg significantly increases the maternal response in experimental animals (increasing number of approaches to the young, reduced latency periods of their translations). For similar changes resulting non-invasive intranasal administration of naloxone (1 mg / kg).
Other researchers also found that naloxone in systemic and central administration leads to strengthening all forms of maternal behavior during the postnatal period, and during early lactation causes an increase in the duration of feeding babies. Therefore, it is advisable to further explore the possibilities of application of naloxone in a situation of maternal depression, the analysis of the prospects for a corresponding expansion of the scope of its practical use.
Thus, the problem of postpartum depression needs to be addressed by acting in two main directions. Firstly, it is necessary to carry out work to explain the importance of early diagnosis of the disease among both mothers and among doctors. And to be most effective would be the realization of a survey of women are not psychiatrists and specialists regularly visit during pregnancy and the postpartum period (eg, gynecologists or pediatricians). Identifying pathologies at an early stage will allow more efficient and perhaps without the use of pharmacological agents to deal with it.
Another topical focus of work is the search for new methods of treatment of maternal depression, in particular, implementation of the fundamentally different from modern antidepressant drug groups. In this regard, it is particularly promising opportunities to study the opioid antagonist naloxone, low-dose estrogen and probably dopamine receptor agonists. Furthermore, in our disposal are still little information on long-term influence on the mother PPD child development. To solve this problem, the creation and analysis of integrated databases of major medical centers.


 Cart
Cart