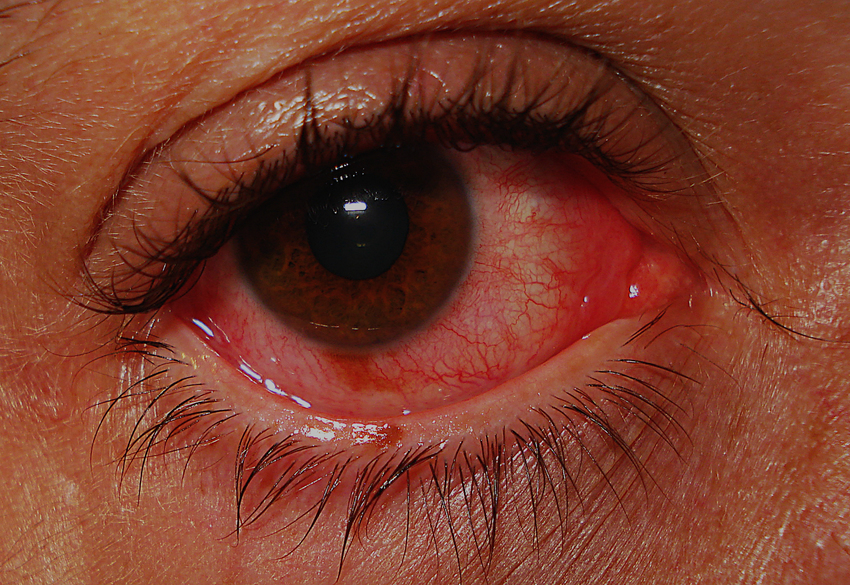
Conjunctivitis. Than to help the inflamed eye?
16 Oct 2018
Reddened eyes, stitched eyelashes, itching and burning as if lodged under the eyelids - here they are, typical symptoms of conjunctivitis, which are able to deliver a sick person a lot of unpleasant sensations. And the longer they last, the higher the risk that acute conjunctivitis will become chronic, and cure it will be much more difficult.
A few words about the problem ...
Conjunctivitis, i.e. inflammation of the connective membrane of the eye, most often occurs as a result of infection (bacterial or viral), allergic reaction, and in some cases under the influence of irritating factors (dust, smoke, contact lenses, etc.).
And although the symptoms of all forms of conjunctivitis are similar, each of them has its own characteristics, which allow one to suspect what triggered the inflammatory process.
So, for example, bacterial conjunctivitis often begins with the defeat of one eye, and only with non-hygiene spreads to the second. It is characterized by abundant mucopurulent discharge, because of which it is difficult for a patient to open his eyes, especially in the morning. Viral conjunctivitis often occurs against the background of a previous acute respiratory viral infection, accompanied by marked reddening of the eyes, lacrimation and photophobia. Allergic conjunctivitis is usually combined with allergic rhinitis, the most pronounced symptoms are itching and burning.
Treatment of conjunctivitis is selected depending on the cause of the disease, the nature of the inflammation (acute, chronic) and accompanying symptoms, but there are several general rules that should be followed in any case. First and foremost, strict hygiene is important: you can only touch the eyes with cleanly washed hands, before the symptoms disappear completely, you must change bed linen (pillowcase) and towel daily, for the instillation of solutions there must be separate pipettes for each eye. Also, careful treatment of the inflamed eye is necessary - mucopurulent discharge should be thoroughly rinsed with a solution of antiseptics (furacilin, ocystistine, potassium permanganate), and not mechanically removed. Drugs in the form of eye drops are usually used during the day, gels and ointments - overnight.
Bacterial conjunctivitis
The main method of treatment of bacterial conjunctivitis is antimicrobial therapy, for which locally acting preparations are used in the form of eye medicinal forms (drops, gels, ointments and films).
Of the antibiotics, the most commonly used drugs are the aminoglycoside group (gentamycin, tobramycin), fluoroquinolones (norfloxacin, ofloxacin), as well as levomycetin, which have a broad spectrum of action and can be used without an exact definition of the causative agent of conjunctivitis.
In some cases, antimicrobial therapy is complemented by the appointment of sulfacetamide, which has a bacteriostatic effect.
If necessary, for example in severe infection, for the treatment of bacterial conjunctivitis, combined drugs are prescribed, which, in addition to the antibiotic, includes a corticosteroid component. These can be preparations based on gentamicin and betamethasone or dexamethasone, neomycin preparations with dexamethasone and polymyxin, as well as drugs of gramicidin with dexamethasone and Framicetin. They have a pronounced anti-inflammatory, antibacterial and antiallergic effect, quickly reduce the acute symptoms of conjunctivitis.
Also, with bacterial conjunctivitis, antiseptics must be used for regular maintenance and treatment of the inflamed eye. The most widely prescribed preparations are decamethoxin, boric acid, zinc sulfate, sodium tetraborate, which have a disinfectant and antiseptic effect. With severe symptoms of inflammation (edema and hyperemia) and contraindications to the use of glucocorticosteroids, antibiotic therapy is supplemented with local forms of NSAIDs, for example, diclofenac preparations in the form of eye drops.
In the acute period of conjunctivitis - the first 3-5 days, antimicrobial drugs (drops) are used every 2-4 hours. After the symptoms of inflammation begin to decrease, the incidence of instillation is reduced to 3-6 times a day. The course of treatment, on average, is 7-10 days.
If the disease was severe, with superficial marginal keratitis, then after the disappearance of acute symptoms, drugs that stimulate the natural mechanisms of regeneration (gel Solcoseril or Actovegin) are prescribed.
Viral conjunctivitis
In most cases, the cause of viral conjunctivitis is adenovirus, the second most common causative agent is the herpes simplex virus - it affects the eyes much less often. On the background of adenovirus infection, inflammation of the conjunctiva develops 2-4 days after the appearance of the first symptoms of acute respiratory viral infection, and proceeds in the form of pharyngoconjunctival fever or epidemic keratoconjunctivitis (more severe form with corneal involvement).
Specific (etiotropaya) therapy with viral conjunctivitis is used today mainly in herpetic infection (acyclovir in the form of an ointment, a solution of idoxuridine). With adenoviral conjunctivitis, antimetabolites (oxoline and tebrofen ointment, florenal ointment) can be used, but their effectiveness leaves much to be desired.
As an alternative to antiviral agents, locally acting interferon preparations (a solution of recombinant interferon alfa-2b) or drugs that stimulate the formation of intrinsic interferons (poludane, aminobenzoic acid) are sometimes prescribed. In general, symptomatic therapy is carried out.
When lesions of the cornea (keratoconjunctivitis) use drugs that improve tissue regeneration: a solution of taurine or retinol acetate, Solcoseryl gel or Actovegin, dexpanthenol, a solution of riboflavin and ascorbic acid.
Antibacterial drugs are not effective against viruses, but in severe viral conjunctivitis, as well as in weakened patients, locally acting drugs of levomycetin, ocystistine, piclosidine may be prescribed to prevent the attachment of a secondary bacterial infection. After the symptoms of acute inflammation begin to subside, a short course of topical glucocorticosteroids (dexamethasone) or combined drugs - corticosteroids and antibiotics (neomycin + dexamethasone + polymixin) is prescribed. If contraindications to the appointment of corticosteroids can be used diclofenac solution.
To reduce painful and uncomfortable sensations, vasoconstrictive drugs (phenylephrine, atropine) can be used - a short course, dazzles (Vidisik, Systein, Oftagel) - for long-term daily use.
Allergic conjunctivitis
Allergic conjunctivitis can be both year-round and seasonal (pollinosis), and in most cases is accompanied by other symptoms of allergy. Therefore, for treatment of all types of allergic conjunctivitis, not only locally acting drugs are used, but also systemic therapy.
With seasonal conjunctivitis, first-line drugs are locally acting antihistamines - azelastine, opatanol, as well as preparations of cromoglycic acid. As a symptomatic therapy, local vasoconstrictors - nafazolinum, diphenhydramine, which are prescribed by short courses (no more than 5 days) are used. With a moderate and severe course of conjunctivitis, corticosteroids are added to the main treatment: eye drops and gels with dexamethasone, hydrocortisone. If allergic inflammation is complicated by the attachment of a bacterial infection, combined drugs (an antibiotic with a corticosteroid) are used.
Systemic therapy is prescribed either in severe pollinosis, or in the case of year-round allergic conjunctivitis, which is resistant to the use of locally acting drugs. In this case, antihistamines of the second generation - ebastine, loratadine, cetirizine, fexofenadine, etc. are prescribed. Alternatively, ketotifen preparations may be used.
With timely treatment and compliance with all medical recommendations, most of the acute conjunctivitis (both infectious and allergic) go without unpleasant consequences and complications within 2-3 weeks. The main thing is not to start the inflammatory process.

 Cart
Cart





